Researcher Zeroes In on Neurological Effects of Long COVID
July 16, 2024 — Neurologic complications from long COVID are widespread, difficult to treat, and often debilitating. These symptoms can resemble a variety of conditions, including some as severe as Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and Postural Orthostatic Tachycardia Syndrome (POTS), making the illness both challenging to diagnose and manage.
New research now suggests long COVID may largely be an autonomic nervous system disorder.
More and more, long COVID patients are reporting symptoms such as intense fatigue, cognitive issues (commonly termed brain fog), dizziness, erratic heart rates, and problems with blood pressure regulation. These are typical hallmarks of dysautonomia, a disorder involving malfunction of the autonomic nervous system.
For many, life may never return to what it once was.
Dr. Lindsay S. McAlpine, a neurologist from Yale School of Medicine and director of the Yale NeuroCOVID Clinic, works with patients still grappling with neurological symptoms long after their infection has seemingly resolved.
"Some patients come in with brain fog and shortness of breath, while others present with palpitations and headaches—it’s a mix of symptoms," McAlpine explained.
Her research is slowly revealing what may lead to a significant breakthrough in treating some of the most elusive long COVID symptoms.
The Role of Vascular Inflammation in Long COVID
The National Institute of Neurological Disorders and Stroke has awarded Dr. McAlpine a 5-year K23 grant to sponsor her ongoing research into “Magnetic Resonance Imaging Biomarkers of Post-COVID-19 Cerebral Microvascular Dysfunction.”
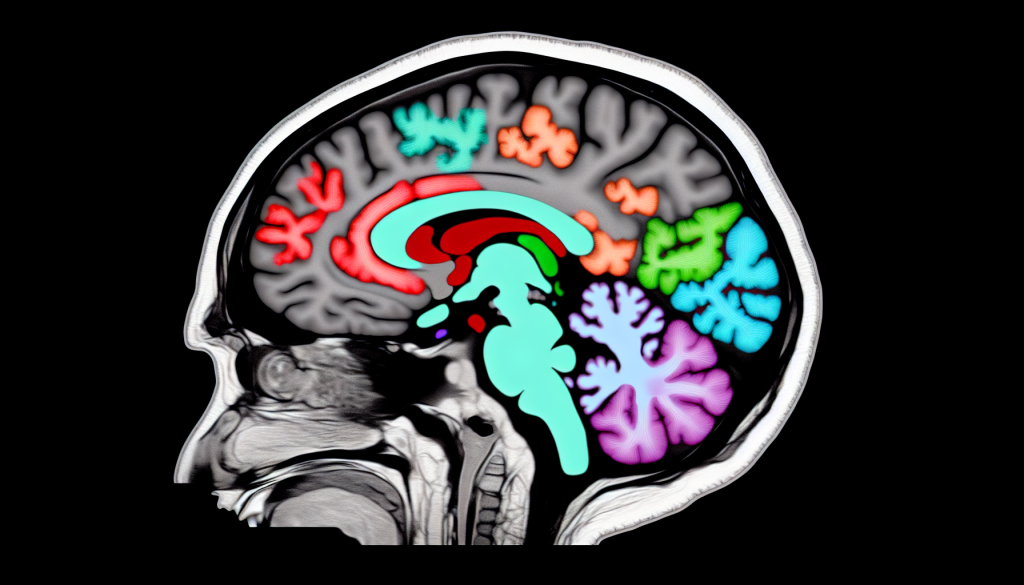
Using advanced MRI techniques, she seeks to uncover biomarkers of microvascular dysfunction in the brain, hoping to shed light on the mechanisms behind post-COVID neurological issues.
“We’re noticing a distinct pattern of vascular inflammation in long COVID that differentiates it from acute COVID. It seems tied to issues with endothelial dysfunction and platelet irregularities,” McAlpine said.
Additionally, her study examines the potential increased risk of small vessel disease due to this dysfunction. The research painstakingly attempts to assemble pieces of the broader pathophysiological puzzle.
“We’re rigorously quantifying cognitive impairments using a 3-hour test battery that helps identify particular deficits in memory and executive function. By combining MRI data, blood analysis, and cognitive tests, we aim to gather important insights,” she added.
McAlpine believes long COVID will eventually be categorized as an autonomic disorder affecting bodily vasculature, with her advanced MRI techniques targeting these intricate connections.
“Several of my MRI protocols center around detecting subtle shifts in blood flow, signaling how different parts of the brain respond to variations in blood demand. Brain fog is a key symptom present not only in long COVID but also in ME/CFS and POTS. My research aims to pinpoint affected brain regions,” she said.
McAlpine’s interest in COVID's neurological effects began early in the pandemic when she noticed an unprecedented rise in ischemic strokes among patients.
“COVID, as it turns out, significantly impacts blood vessels, contributing to vascular inflammation. We were seeing stroke cases uncommon in viral infections,” she noted.
After observing these cases, McAlpine began investigating, eventually uncovering widespread endotheliopathy—damage to the blood vessel lining—that led to clot formation and dysfunction.
Unraveling a Complex Set of Neuropsychiatric Symptoms
At the Demystifying Long COVID North American Conference 2024, held in Boston this June, McAlpine presented her work on long COVID’s complex neuropsychiatric impacts. These range from cognitive issues and headaches to neuropathy, mental health challenges, and dysautonomia.
“While there are many overlapping symptoms that mix and match across long COVID patients, I wanted to isolate one—brain fog and cognitive impairment—that clearly originates in the brain,” she said.
In September 2021, Translational Psychiatry published a study on COVID-19’s neuropsychiatric symptoms, offering possible mechanisms and therapeutic strategies. Even in the early days of the pandemic, confusion, delirium, and neurocognitive disorders were reported, puzzling healthcare professionals who initially expected more respiratory complaints.
The study demonstrated that the coronavirus could invade the central nervous system, leading to brain injury and disruption to key brainstem function, including the cardiorespiratory center.
Imaging and chemical evidence from the research showed neuroimmune dysfunction and brain damage in severely affected patients. The proposed treatments included immunosuppressive therapies, vaccines targeting the virus’s spike protein, and drugs aimed at improving vascular integrity.
However, much remained unknown, and the research emphasized the need for future multi-disciplinary exploration.
The Link Between Immune Dysfunction and Long COVID
Similarly, McAlpine and her team continue to try and untangle the web of immune dysfunction that seems to accompany long COVID.
A study released in April revealed that post-COVID small fiber neuropathy (SFN) may be immune-mediated, indicating an underlying immune dysfunction as the culprit.
Interestingly, researchers noted that SFN could be a pathological hallmark of long COVID, having previously been associated with both ME/CFS and POTS. The prevailing theory suggests an exaggerated immune response to viral infections could trigger immune system irregularities, ultimately damaging small fiber nerves.
That said, unresolved questions abound.
“We’ve observed quite a bit of immune dysfunction, but there’s still so much we don’t understand,” McAlpine acknowledged. “I’m especially curious about how autonomic dysfunction and immune dysregulation are interconnected, and how this correlates with vascular inflammation,” she added.
Still, not all long COVID patients exhibit autoimmune dysfunction, which complicates the search for common biomarkers.
“When diagnosing neuroinfectious or autoimmune diseases like multiple sclerosis, spinal fluid reveals clear signs of inflammation—elevated white blood cells, proteins, and antibodies. But with long COVID patients, the picture is quite different," she explained.
Untangling the intricate relationships between immune, vascular, and neurological factors remains a formidable challenge, and there may not be a singular answer for everyone.
“It’s all about that intersection of the immune system and blood vessels. The next steps are determining precise treatment targets, but with such diverse presentations among patients, it’s an ongoing puzzle,” McAlpine said.
Treatment Options Physicians Can Use Now
While a definitive cure remains elusive, there is emerging evidence that a combination of N-acetyl cysteine (NAC) and guanfacine could alleviate some neurological symptoms.
In a small study published in Neuroimmunology Reports in November 2023, Yale behavioral neurologist Dr. Arman Fesharaki-Zadeh and neuroscientist Dr. Amy Arnsten offered early insights. Their research, involving 12 patients, showed that daily doses of 600 mg NAC and 1 mg (eventually 2 mg) guanfacine significantly improved cognitive function in most participants.
Notably, working memory, executive function, and concentration showed improvement, with some patients returning to their regular work schedules—something often disrupted by long COVID.
Although larger placebo-controlled trials are necessary, the study has established the treatment’s safety and opened doors for more extensive investigation. NAC is available over the counter, and patients can obtain guanfacine off-label with a prescription.
Dr. McAlpine has also seen promising results from using this combination in her patients at the NeuroCOVID clinic.
In addition to medications, lifestyle changes—such as reducing tobacco and alcohol intake, increasing physical and mental exercise, and taking vitamin D supplements (1000-2000 IU daily)—may also help manage persistent brain fog.
Vitamin D plays a crucial role in supporting brain health by reducing aging biomarkers in the brain, regulating critical genes, activating enzymes responsible for neurotransmitter production, and promoting neuron growth and survival.